Blog
An alarming rise in benzodiazepine-related morbidity and mortality is a growing concern in the U.S., research has concluded that 919 benzodiazepine ambulatory visits occurred in 2003 and increased drastically to 1672 in 2015.1 The reported ambulatory visits have resulted in a 127 percent increase in benzodiazepine-related deaths or injuries. Amid the opioid crisis, benzodiazepine use/abuse is significantly growing with more than 30 percent of overdoses involving opioids also involve benzodiazepines.2
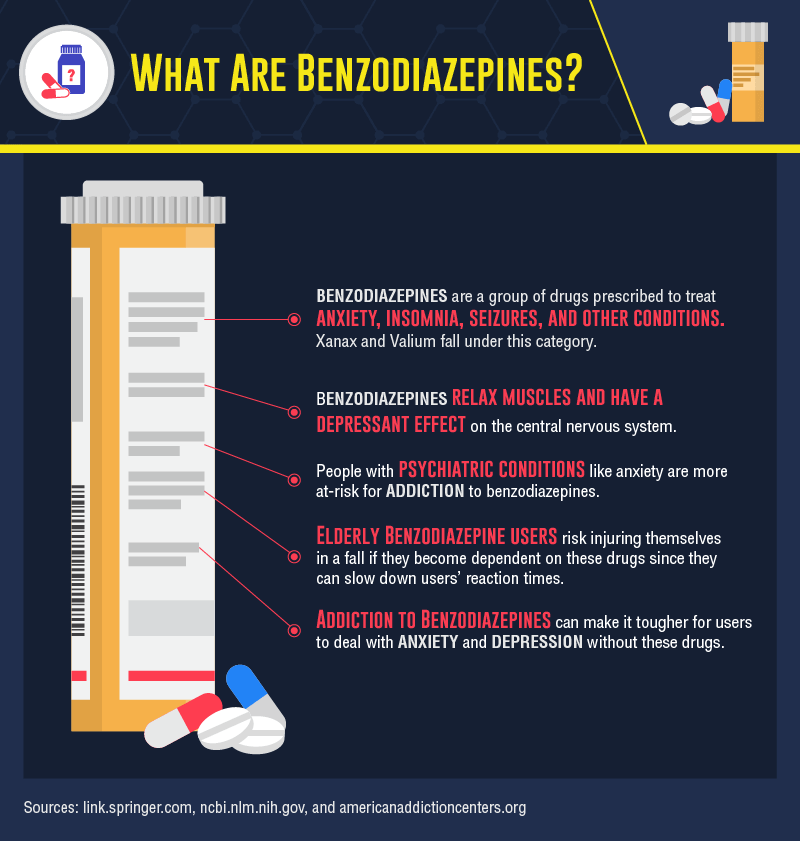
To provide a better understanding of how powerful benzodiazepines are, the medical realm has defined the substance as a tranquilizer that acts on the central nervous system producing sedation and muscle relaxation. The following benzodiazepines are classified by their length of effect:
- Ultra Short Acting-Midazolam (Versed®) and Triazolam (Halcion®)
- Short Acting- Alprazolam (Xanax®) and Lorazepam (Ativan®)
- Long Acting-Chlordiazepoxide (Librium®) and Diazepam (Valium®)3
According to a 2018 study, 30 million Americans used benzodiazepines in the past year and of those more than 5 million misused them for purposes of a sleep aid or to get high.4 Benzodiazepines can lead to physical and psychological dependence. In fact, high doses of benzodiazepines can create signs and symptoms of acute toxicity or overdose including drowsiness, confusion, dizziness, blurred vision, weakness, slurred speech, difficulty breathing and even coma.3
Despite the risks associated with benzodiazepines, research and statistics are finding that there has been a spike in prescribing in lieu of the opioid crisis. A study from 2003-2015 indicated a substantial increase of primary care physicians (PCP’s) who are issuing prescriptions for benzodiazepines-3.6 percent to 7.5 percent.1 Primary care physicians defined by the National Ambulatory Medical Care Survey (NAMCS) includes: family medicine, internal medicine, geriatric medicine and obstetrics and gynecology. The increased number of benzodiazepine visits suggests there is a growing number of patients being prescribed this drug, along with prescriptions written for long-term use.
In 2015, 23 percent of people who died of an opioid overdose also tested positive for benzodiazepines.2 In a 2016 study, researchers noted that when opioids and benzodiazepines are used simultaneously, a 570 percent increase in substance abuse treatment admissions occurred.4 Co-prescribing, which is defined as prescribing two or more drugs to the same patient is an apparent, yet overlooked contributing factor to the drug epidemic we are facing today.
In 2015, benzodiazepines were co-prescribed with an opioid in 19.2 percent of visits, opioids were co-prescribed with a benzodiazepine in 26.4 percent of visits.1 As opioids lose favor among prescribers, it is imperative to be aware of the risks that are associated with benzodiazepines, especially when used in combination with an opioid. It is strongly advised that clinicians avoid prescribing benzodiazepines concurrently with opioids.
In 2016, the FDA required benzodiazepines to be “black box” labeled in efforts to warn patients about the drug’s side effects and the heightened risks when taken with opioids. As a Schedule III drug, benzodiazepines have an increased probability for dependency. Physicians are advised to prescribe with caution, to fully inform their patients of the risks involved with benzodiazepines and the threat of fatality when combined with an opioid.
Utilizing advanced drug testing, specifically for benzodiazepines can be a proactive approach in identifying potential at-risk behavior and preventing fatal outcomes. Advanced drug testing uses different specimen types to detect substances of abuse at different times. Depending on the specimen’s window of detection, short-term and long-term use can be identified as the following:
Short-Term:
- Urine- 2-3 days
- Oral Fluid-1-2 days
- Blood-1-2 days
Long-Term:
- Hair- 3 months
- Fingernail-3-6 months
Utilizing an accredited laboratory that offers extensive panels to test for drugs of abuse is imperative in counteracting the impending drug crisis of benzodiazepines.
Benzodiazepines in Hair Benzodiazepines in Nail
Benzodiazepines in ChildGuard Benzodiazepines in Urine
References:
- Agarwal, S. D. (2019, January 25). Patterns in Outpatient Benzodiazepine Prescribing in the United States. Retrieved from https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2722576
- National Institute on Drug Abuse. (2018, March 15). Benzodiazepines and Opioids. Retrieved from https://www.drugabuse.gov/drugs-abuse/opioids/benzodiazepines-opioids
- Benzodiazepine Abuse. (n.d.). Retrieved from https://www.webmd.com/mental-health/addiction/benzodiazepine-abuse
- Smith, M. (2019, February 06). After Opioids, Benzodiazepine Use Raises Concern. Retrieved from https://nida.nih.gov/research-topics/opioids/benzodiazepines-opioids
- Forensic vs. Clinical Drug Testing: Why Flexibility Matters for Your Organization
- USDTL’s Integration and Partnership With CourtFact
- New Year, New Capabilities: Offering Forensic & Clinical Testing Options
- Weather Delay
- The Detection of Delta-9-tetrahydrocannabinol, Delta-8-tetrahydrocannabinol, Delta-10-tetrahydrocannabinol, and Cannabidiol in Hair Specimens
- Umbilical Cord Tissue Testing for Ketamine
- Drugs of Abuse: A DEA Resource Guide (2024)
- Beyond THC and CBD: Understanding New Cannabinoids
- February 2026 (1)
- January 2026 (3)
- October 2025 (1)
- July 2025 (3)
- May 2025 (2)
- April 2025 (2)